Which Technique Should Should the Practical Nurse to Give a Z-track
Part 1 of this two-part series on injection techniques describes the evidence base and procedure for administering an intramuscular injection
Abstract
The intramuscular route allows the rapid absorption of drugs into the circulation. Using the correct injection technique and selecting the correct site will minimise the risk of complications. This is part 1 of a two-part series on injection techniques. Part 2 covers the subcutaneous route.
Citation: Shepherd E (2018) Injection technique 1: administering drugs via the intramuscular route. Nursing Times [online]; 114: 8, 23-25.
Author: Eileen Shepherd is clinical editor at Nursing Times.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- Read part 2 of this series here
Introduction
Drugs administered by the intramuscular (IM) route are deposited into vascular muscle tissue, which allows for rapid absorption into the circulation (Dougherty and Lister, 2015; Ogston-Tuck, 2014).
Complications of poorly performed IM injection include:
- Pain – strategies to reduce this are outlined in Box 1;
- Bleeding;
- Abscess formation;
- Cellulitis;
- Muscle fibrosis;
- Injuries to nerves and blood vessels (Small, 2004);
- Inadvertent intravenous (IV) access.
These complications can be avoided if the site for injection is accurately identified and a skilled evidence-based technique is used (Greenway, 2014).
Box 1. How to reduce pain caused by injection technique
- Use the correct technique
- Rotate injection site to prevent indurations or abscesses
- Explain the benefits of the injection to the patient
- Position the patient so the muscles are relaxed
- Use distraction
- Insert and remove the needle smoothly and quickly
- Hold the syringe steady during the procedure
- Inject medication slowly but smoothly
Source: Dougherty and Lister (2015)
Evidence base
The procedure for IM injection has been discussed widely in the literature but there are concerns that nurses are still performing outdated and ritualistic practice relating to site selection, aspirating back on the syringe (Greenway, 2014) and skin cleansing.
Site selection
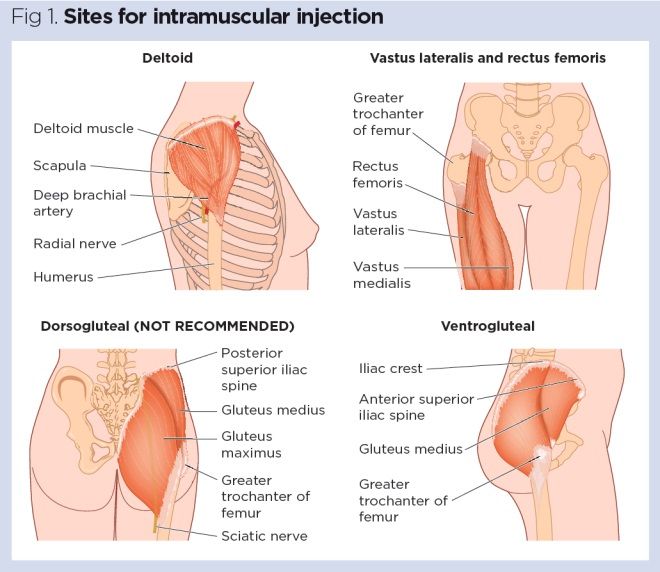
Four muscle sites are recommended for IM administration (Fig 1, Table 1):
- Vastus lateralis;
- Rectus femoris
- Deltoid;
- Ventrogluteal.
Traditionally the dorsogluteal (DG) muscle was used for IM injections but this muscle is in close proximity to a major blood vessel and nerves, with sciatic nerve injury a recognised complication (Small, 2004). In addition, drug absorption from the DG muscle may be slower than other sites and this can lead to a build-up of drugs in the tissues and risk of overdose (Malkin, 2008). Many patients find the use of the DG site intrusive and are reluctant to undress to give access to the relevant area. For these reasons, the DG muscle is no longer recommended for IM injections – in spite of this, many nurses continue to use it (Ogston-Tuck,2014; Walsh and Brophy, 2011; Malkin, 2008).

Needles
Safety needles should be used for IM injections to reduce the risk of needle-stick injury (Health and Safety Executive, 2013).
Needle size is measured in gauges (diameter of the needle). A 21G is commonly used but selection depends on the viscosity of the liquid being injected (Dougherty and Lister, 2015). Public Health England (2013) recommends 23G or 25G needle for IM vaccines.
Needles need to be long enough to ensure the drug is injected into the muscle; length depends on:
- Muscle mass;
- Patient's weight;
- Amount of subcutaneous fat.
Women have more subcutaneous fat than men (Zaybak et al, 2007) and consideration needs to be given to using longer needles for patients who are obese. PHE (2013) recommends that a 25mm or 38mm needle is used in adults.
Traditionally nurses have been taught to leave a few millimetres between the skin and the hub of the needle in case the needle breaks off during the injection. This practice is not evidence based, may cause medication to be delivered into the subcutaneous fat layer and, with modern single-use needles, is no longer necessary (Greenway, 2014).
Skin preparation
There is some debate about using alcohol-impregnated swabs to clean injection sites. PHE (2013) suggests that, if a patient is physically clean and generally in good health, swabbing the skin is not required.
In older or immunocompromised patients, skin preparation using an alcohol-impregnated swab may be recommended (70% isopropyl alcohol) (Dougherty and Lister, 2015). Follow local policy.
Aspiration
It is common practice to draw back on a syringe after the needle is inserted to check whether it is in a blood vessel. While it is important to aspirate if the DG muscle site is used – because of proximity to the gluteal artery – it is not required for other IM injection sites (PHE, 2013; Malkin, 2008).
Gloves
The World Health Organization (2010, 2009) states that gloves need not be worn for this procedure if the health worker's and patient's skin are intact. It also notes that gloves do not protect against needle-stick injury. Nurses need to risk assess individual patients (Royal College of Nursing, 2018) and be aware of local policies for glove use.
Equipment
- Needles – one of which should be a safety-engineered device;
- Syringe;
- Drug for administration;
- Medicines administration chart/prescription;
- Receiver or tray to carry the drug;
- Sharps container.
Procedure
- Explain the procedure and gain consent.
- Screen the patient to ensure privacy during the procedure.
- Before drug administration, check whether the patient has any allergies.
- Check the prescription is correct, following the 'five rights' of drug administration (Box 2) and local medicines administration policy to reduce the risk of error.
- Wash and dry hands to reduce the risk of infection.
- Assemble the syringe and needle, and withdraw the required amount of drug from the ampoule. Some medicines are available in pre-filled syringes and manufacturer's instructions should be followed.
- Disperse air bubbles from the syringe.
- Change the needle. Doing so will ensure that the needle used for the injection is sharp, thereby reducing pain (Agac and Günes, 2011). A safety-engineered needle should be used as this reduces the risk of sharps injury.
- Dispose of the used needle in a sharps container according to local policy.
- Place the filled syringe in a tray and take it to the patient, along with a sharps bin so the used sharps can be disposed of immediately after the procedure.
- Check the patient's identity, according to local medicines management policy.
- Position the patient comfortably with the injection site exposed (Fig 1). The site is influenced by the assessment of the patient, the drug and the volume to be injected (Table 1) (Dougherty and Lister, 2015).
- Check the site for signs of oedema, infection or skin lesions. If any of these are present, select a different site.
- Wash and dry hands.
- If gloves are considered necessary, following the risk assessment, these should be applied.
- Ensure the skin is clean and follow local policy on skin cleansing.
- If skin cleansing is considered necessary, swab for 30 seconds with isopropyl alcohol and allow to dry for 30 seconds (Dougherty and Lister, 2015).
- Inform the patient you are going to carry out the procedure. Use distraction and relaxation techniques to reduce pain if needed (Box 1).
- Hold the syringe and needle in your dominant hand and gently stretch the skin around the injection site using the non-dominant hand. This displaces the subcutaneous tissue and aids needle entry (Dougherty and Lister, 2015).
- A Z-track technique can be used to prevent backtracking and leakage from the injection site (Fig 2).
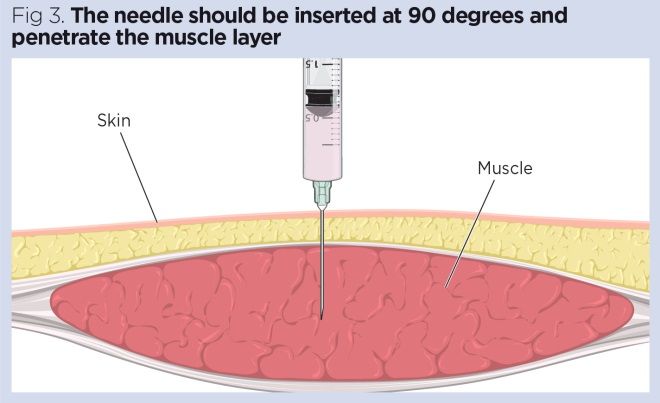
- Insert the needle at a 90-degree angle using a dart-like action. This prevents accidental depression of the plunger during insertion of the needle (Malkin, 2008) (Fig 3).
- Aspiration to check whether the needle is in a blood vessel is not usually necessary (PHE, 2013). Aspiration is only required when the DG site is used, which is not recommended (Greenway, 2014; Malkin, 2008).
- Depress the plunger slowly at a rate of 1ml/10 seconds; this aids absorption of the drug and reduces pain (Dougherty and Lister, 2015).
- Wait for 10 seconds to allow the drug to diffuse into the tissue and then quickly withdraw the needle (Dougherty and Lister, 2015).
- Dispose of the sharps directly into the sharps bin and the syringe according to local policy.
- Ensure the patient is comfortable and wash your hands.
- Record administration on the prescription chart, as well as the administration site as repeated injections into the same site can lead to induration and abscesses.
- Monitor the patient for any effects of the prescribed medicine and any problems with the injection site.
Box 2. 'Five rights' of medicines administration
- Right patient
- Right drug
- Right time
- Right dose
- Right route

Ağaç E, Güneş UY (2011) Effect on pain of changing the needle prior to administering medicines intramuscularly: a randomized controlled trial. Journal of Advanced Nursing; 67: 3, 563-568.
Dougherty L, Lister S (2015) The Royal Marsden Hospital Manual of Clinical Nursing Procedures. Oxford: Wiley-Blackwell.
Greenway K (2014) Rituals in nursing: intramuscular injection. Journal of Clinical Nursing; 23: 23-24, 3583-3588.
Health and Safety Executive (2013) Health and Safety (Sharp Instruments in Healthcare) Regulations 2013: Guidance for Employers and Employees.
Malkin B (2008) Are techniques used for intramuscular injection based on research evidence? Nursing Times; 104: 50/51, 48-51.
Ogston-Tuck S (2014) Intramuscular injection technique: an evidence-based approach. Nursing Standard; 29: 4, 52-59.
Public Health England (2013) Immunisation Procedures: The Green Book, Chapter 4.
Royal College of Nursing (2018) Tools of the Trade: Guidance for Health Care Staff on Glove Use and the Prevention of Contact Dermatitis.
Small SP (2004) Preventing sciatic nerve injury from intramuscular injections: literature review. Journal of Advanced Nursing; 47: 3, 287-296.
Walsh L, Brophy K (2011) Staff nurses' sites of choice for administering intramuscular injection to adult patients in the acute care setting. Journal of Advanced Nursing; 67: 5, 1034-1040.
World Health Organization (2010) WHO Best Practices for Injections and Related Procedures Toolkit.
World Health Organization (2009) WHO Guidelines on Hand Hygiene in Health Care.
Zaybak A et al (2007) Does obesity prevent the needle from reaching muscle in intramuscular injections? Journal of Advanced Nursing; 58: 6, 552-556.
Which Technique Should Should the Practical Nurse to Give a Z-track
Source: https://www.nursingtimes.net/clinical-archive/assessment-skills/injection-technique-1-administering-drugs-via-the-intramuscular-route-23-07-2018/
0 Response to "Which Technique Should Should the Practical Nurse to Give a Z-track"
Post a Comment